AI Medical Necessity Platform
Correct ICD & CPT Codes in Minutes — Even for Millions of Patients
The Problem Finding Medical Necessities Individually create Real problems
Every Patient needs manual ICD research
- Provider must look up medical necessity code patient-by-patient
- Take 5-15 mints per patient just to identify qualified patient and confirm ICD coverage
- No standard process – every provider does it differently
High risk of missing required ICD-Code/Documentation/Coverage
- Manual approach often missed secondary & combined ICD codes
- Unsupported ICD – Claim denial
- Partial ICD selection = Loss of revenue
- No guarantee that medical necessity criteria is fully captured
Denied claims mean big Financial loss
- Missing 1 ICD can cause complete claim rejection
- Resubmitting takes weeks
- Provider must appeal manually
- Cash flow impact – Delayed reimbursement
No Payer logic or LCD guidance
- Provider often select ICD without payer-specific LCD rules
- Every payer has different rules
- Manual process can not track payer rules
- Audit exposure increase
Compliance Risk
- If medical necessity if not fully documented;
- Audit fines
- Claw backs
- Legal exposure
- Documentation Gap

WT - AI Solution Platform
Our AI Medical Necessity Engine
- Accurate idenfies all medically necessary ICD Codes in seconds
- Learn clinic-specific coding patterns based on provider preference
- Scan millions of patient records in minutes for population-level optimization
- Generate fully Audit-proof documentation logic for every claim
Patient-Level Intelligence
- Can research a single patient and identify medical necessity based on:
- Provider treatment approach
- Clinical notes and exam findings
- Patient history, symptoms, progress notes, intake forms, Lab result
- Benefits to the patient and medical standard of care
- Automatically identifies secondary ICD codes that support the medical necessity
- Help provider understand why the test is required, not just what code to use
HIPAA & Compliance
- End to end HIPAA compliant architecture
- NO PHI is stored outside secure boundaries
- Structured audit trail for every ICD logic decision
- Ensure claims are legally defensible in an audit
- Generate fully Audit-proof documentation logic for every claim
Provider-Focused customization
- Can adjust recommendation based on Clinic requirements (e.g. ANS is diabetic neuropathy vs orthostatic hypotension vs, syncope cases)
- Support individual decision-making per patient
- Saves time spent researching ICD-justification
- Work for small clinics + multi-location groups
Dashboard & Analytics
- Customer clinic dashboard for providers:
- Daily patient volumes (Number of eligible medical necessity patients)
- ICD utilization trends
- Customization as per provider requirement

Key Features
AI & Medical
Necessity Engine
-
scorecard
Multi-clinic analytic
dashboards
Clinical decision support to guide accurate decision rules
Identifies secondary ICDs bases on history, symptoms and combination
Multi-diagnostic support – ANS, LAB, Echo, Ultrasound etc.
HIPAA-compliant architecture
Clinical value & patient benefits
EMR/EHR
integration
Automatic audit documentation
ICD/CPT code Suggestion
Reduces denials & improves reimbursement
Scan to millions of patients records in minutes

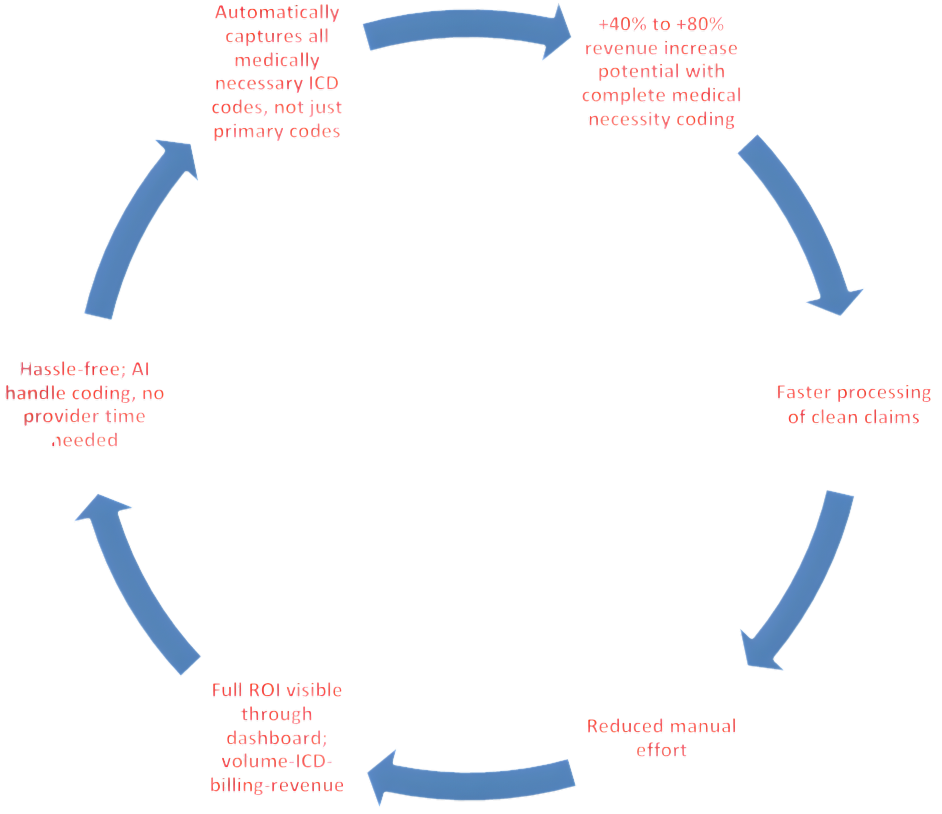
Revenue Impact